Treatment
Impulsive type
At least three of the following must be present, one of which must be (2):
1. marked tendency to act unexpectedly and without consideration of the consequences;
2. marked tendency to engage in quarrelsome behavior and to have conflicts with others, especially when impulsive acts are thwarted or criticized;
3. liability to outbursts of anger or violence, with inability to control the resulting behavioral explosions;
4. difficulty in maintaining any course of action that offers no immediate reward;
5. unstable and capricious (impulsive, whimsical) mood.


Borderline type
At least three of the symptoms mentioned in Impulsive type must be present see above, with at least two of the following in addition:
1. disturbances in and uncertainty about self-image, aims, and internal preferences;
2. liability to become involved in intense and unstable relationships, often leading to emotional crisis;
3. excessive efforts to avoid abandonment;
4. recurrent threats or acts of self-harm;
5. chronic feelings of emptiness.
6. demonstrates impulsive behavior, e.g., speeding in a car or substance abuse
The ICD-10 also describes some general criteria that define what is considered a Personality disorder.
Millon's subtypes
Theodore Millon has proposed four subtypes of BPD. He suggests that an individual diagnosed with BPD may exhibit none, one, or more of the following:

Subtype | Features |
|---|---|
Discouraged (including avoidant or dependent personality features) |
Pliant, submissive, loyal, humble; feels vulnerable and in constant jeopardy; feels hopeless, depressed, helpless, and powerless. |
Petulant (including negativistic features) |
Negativistic, impatient, restless, as well as stubborn, defiant, sullen, pessimistic, and resentful; easily feels "slighted" and quickly disillusioned. |
Impulsive (including histrionic or antisocial features) |
Capricious, superficial, flighty, distractible, frenetic, and seductive; fearing loss, the individual becomes agitated; gloomy and irritable; and potentially suicidal. |
Self-destructive (including depressive or masochistic and self-defeating features) |
Inward-turning, intropunitively (self-punishing) angry; conforming, deferential, and ingratiating behaviors have deteriorated; increasingly high-strung and moody; possible suicide. |
Misdiagnosis
People with BPD may be misdiagnosed for a variety of reasons. One reason for misdiagnosis is BPD has symptoms that coexist (comorbidity) with other disorders such as depression, PTSD, and bipolar disorder.Family members
People with BPD are prone to feeling angry at members of their family and alienated from them. On their part, family members often feel angry and helpless at how their BPD family members relate to them. Parents of adults with BPD are often both over-involved and under-involved in family interactions. In romantic relationships, BPD is linked to increased levels of chronic stress and conflict, decreased satisfaction of romantic partners, abuse, and unwanted pregnancy. However, these links may apply to personality disorders in general.Adolescence
Onset of symptoms typically occurs during adolescence or young adulthood, although symptoms suggestive of this disorder can sometimes be observed in children. Symptoms among adolescents that predict the development of BPD in adulthood may include problems with body-image, extreme sensitivity to rejection, behavioral problems, non-suicidal self-injury, attempts to find exclusive relationships, and severe shame. Many adolescents experience these symptoms without going on to develop BPD, but those who experience them are 9 times as likely as their peers to develop BPD. They are also more likely to develop other forms of long-term social disabilities. Clinicians are discouraged from diagnosing anyone with BPD before the age of 18, due to the normal ups and downs of adolescence and a still-developing personality. However, BPD can sometimes be diagnosed before age 18, in which case the features must have been present and consistent for at least one year.A BPD diagnosis in adolescence might predict that the disorder will continue into adulthood. Among adolescents who warrant a BPD diagnosis, there appears to be one group in which the disorder remains stable over time and another group in which the individuals move in and out of the diagnosis. Earlier diagnoses may be helpful in creating a more effective treatment plan for the adolescent. Family therapy is considered a helpful component of treatment for adolescents with BPD.
Differential diagnosis and comorbidity
Lifetime comorbid (co-occurring) conditions are common in BPD. Compared to those diagnosed with other personality disorders, people with BPD showed a higher rate of also meeting criteria for
- mood disorders, including major depression and bipolar disorder
- anxiety disorders, including panic disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD)
- other personality disorders
- substance abuse
- eating disorders, including anorexia nervosa and bulimia
- attention deficit hyperactivity disorder
- somatic symptom disorder (formerly known as a somatoform disorder, this is a category of mental disorder included in a number of diagnostic schemes of mental illness)
- dissociative disorders
A diagnosis of a personality disorder should not be made during an untreated mood episode/disorder, unless the lifetime history supports the presence of a personality disorder.
Comorbid Axis I disorders
Gender differences in Axis I lifetime comorbid diagnosis, 2008 and 1998 |
|||
Axis I diagnosis |
Overall (%) |
Male (%) |
Female (%) |
Mood disorders |
75.0 |
68.7 |
80.2 |
Major depressive disorder |
32.1 |
27.2 |
36.1 |
Dysthymia |
9.7 |
7.1 |
11.9 |
Bipolar I disorder |
31.8 |
30.6 |
32.7 |
>Bipolar II disorder |
7.7 |
6.7 |
8.5 |
Anxiety disorders |
74.2 |
66.1 |
81.1 |
Panic disorder with agoraphobia |
11.5 |
7.7 |
14.6 |
Panic disorder without agoraphobia |
18.8 |
16.2 |
20.9 |
Social phobia |
29.3 |
25.2 |
32.7 |
Specific phobia |
37.5 |
26.6 |
46.6 |
PTSD> |
39.2 |
29.5 |
47.2 |
>Generalized anxiety disorder |
35.1 |
27.3 |
41.6 |
Obsessive-compulsive disorder** |
15.6 |
--- |
--- |
Substance use disorders |
72.9 |
80.9 |
66.2 |
Any alcohol use disorder |
57.3 |
71.2 |
45.6 |
Any drug use disorder |
36.2 |
44.0 |
29.8 |
Eating disorders** |
53.0 |
20.5 |
62.2 |
>Anorexia nervosa** |
20.8 |
7 * |
25 * |
>Bulimia nervosa** |
25.6 |
10 * |
30 * |
Eating disorder not otherwise specified** |
26.1 |
10.8 |
30.4 |
Somatoform disorders** |
10.3 |
10 * |
10 * |
Somatization disorder** |
4.2 |
--- |
--- |
Hypochondriasis** |
4.7 |
--- |
--- |
Somatoform pain disorder** |
4.2 |
--- |
--- |
Psychotic disorders** |
1.3 |
1 * |
1 * |
* Approximate values |
|||
A 2008 study found that at some point in their lives, 75 percent of people with BPD meet criteria for mood disorders, especially major depression and Bipolar I, and nearly 75 percent meet criteria for an anxiety disorder Nearly 73 percent meet criteria for substance abuse or dependency, and about 40 percent for PTSD. It is noteworthy that less than half of the participants with BPD in this study presented with PTSD, a prevalence similar to that reported in an earlier study. The finding that less than half of patients with BPD experience PTSD during their lives challenges the theory that BPD and PTSD are the same disorder. There are marked gender differences in the types of comorbid conditions a person with BPD is likely to have a higher percentage of males with BPD meet criteria for substance-use disorders, while a higher percentage of females with BPD meet criteria for PTSD and eating disorders. In one study, 38% of participants with BPD met the criteria for a diagnosis of ADHD. In another study, 6 of 41 participants (15%) met the criteria for an autism spectrum disorder (a subgroup that had significantly more frequent suicide attempts). Regardless that it is an infradiagnosed disorder, a few studies have shown that the "lower expressions" of it might lead to wrong diagnoses. The many and shifting Axis I disorders in people with BPD can sometimes cause clinicians to miss the presence of the underlying personality disorder. However, since a complex pattern of Axis I diagnoses has been found to strongly predict the presence of BPD, clinicians can use the feature of a complex pattern of comorbidity as a clue that BPD might be present.
Psychotherapy
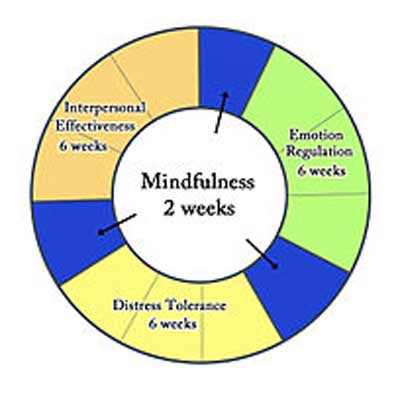
The stages used in dialectical behavior therapy.
Long-term psychotherapy is currently the treatment of choice for BPD. More rigorous treatments are not substantially better than less rigorous treatments. There are six such treatments available: dynamic deconstructive psychotherapy (DDP), mentalization-based treatment (MBT), transference-focused psychotherapy, dialectical behavior therapy (DBT), general psychiatric management, and schema-focused therapy. While DBT is the therapy that has been studied the most, all these treatments appear effective for treating BPD, except for schema-focused therapy. Long-term therapy of any kind, including schema-focused therapy, is better than no treatment, especially in reducing urges to self-injure.
Cognitive behavioral therapy (CBT) is also a type of psychotherapy used for treatment of BPD. This type of therapy relies on changing people's behaviors and beliefs by identifying problems from the disorder. CBT is known to reduce some anxiety and mood symptoms as well as reduce suicidal thoughts and self-harming behaviors.
Mentalization-based therapy and transference-focused psychotherapy are based on psychodynamic principles, and dialectical behavior therapy is based on cognitive-behavioral principles and mindfulness. General psychiatric management combines the core principles from each of these treatments, and it is considered easier to learn and less intensive. Randomized controlled trials have shown that DBT and MBT may be the most effective, and the two share many similarities. However, a naturalistic study indicated that DDP may be more effective than DBT. Researchers are interested in developing shorter versions of these therapies to increase accessibility, to relieve the financial burden on patients, and to relieve the resource burden on treatment providers.
From a psychodynamic perspective, a special problem of psychotherapy with people with BPD is intense projection. It requires the psychotherapist to be flexible in considering negative attributions by the patient rather than quickly interpreting the projection.
Some research indicates that mindfulness mation may bring about favorable structural changes in the brain, including changes in brain structures that are associated with BPD.
Because of weak evidence and the potential for serious side effects from some of these medications, the UK National Institute for Health and Clinical Excellence (NICE) 2009 clinical guideline for the treatment and management of BPD recommends, "Drug treatment should not be used specifically for borderline personality disorder or for the individual symptoms or behavior associated with the disorder." However, "drug treatment may be considered in the overall treatment of comorbid conditions." They suggest a "review of the treatment of people with borderline personality disorder who do not have a diagnosed comorbid mental or physical illness and who are currently being prescribed drugs, with the aim of reducing and stopping unnecessary drug treatment."