Other Addictions
Sexual addiction
Sexual addiction, also known as sex addiction, is a state characterized by compulsive participation or engagement in sexual activity, particularly sexual intercourse, despite negative consequences.5 Proponents of a diagnostic model for sexual addiction, as defined here, consider it to be one of several sex-related disorders within an umbrella concept known as hypersexual disorder.6 In clinical diagnostics, the term sexual dependence may also refer to a conceptual model that is used to assess people who report being unable to control their sexual urges, behaviors, or thoughts. Related models of pathological sexual behavior include hypersexuality (nymphomania and satyriasis), erotomania, Don Juanism (or Don Juanitaism), and paraphilia-related disorders.
Clinicians, such as psychiatrists, sociologists, sexologists, and other specialists, have differing opinions on the classification and clinical diagnosis of sexual addiction. As a result, "sexual addiction" does not exist as a clinical entity in either the DSM or ICD medical classifications of diseases and medical disorders. Neuroscientists, pharmacologists, molecular biologists, and other researchers in related fields have identified a transcriptional and epigenetic model of drug and behavioral (including sexual) addiction pathophysiology. Diagnostic models, which use the pharmacological model of addiction (this model associates addiction with drug-related concepts, particularly physical dependence, drug withdrawal, and drug tolerance),10 do not currently include diagnostic criteria to identify sexual addictions in a clinical setting. In the alternative reward-reinforcement model of addiction, which uses neuropsychological concepts to characterize addictions, sexual addictions are identifiable and well-characterized.1112 In this model, addictive drugs are characterized as those which are both reinforcing and rewarding (i.e., activates neural pathways associated with reward perception). Addictive behaviors (those which can induce a compulsive state) are similarly identified and characterized by their rewarding and reinforcing properties.

Current research on sexual addiction within the context of the reward-reinforcement model indicates that it is well-characterized as an addiction1112 and that it develops through the same biomolecular mechanisms that induce drug addictions. Specifically, sexual activity is an intrinsic reward that has been shown to act as a positive reinforcer, strongly activate the reward system, and induce the accumulation of ΔFosB in part of the striatum (specifically, the nucleus accumbens). Chronic and excessive activation of certain pathways within the reward system and the accumulation of ΔFosB in a specific group of neurons within the nucleus accumbens has been directly implicated in the development of the compulsive behavior that characterizes addiction.
3 hospice 3factor model
Accepted research now shows that some people have vulnerabilities to addiction and has established a three-factor standard for vulnerability to drug addiction: genetic factors, environmental factors and repeated exposure to drugs of abuse. Being vulnerable to addiction means that there exists some factor which makes one individual more likely to develop an addiction than another individual. Additionally, many in the science community agree that addiction is not simply just a result of desensitized neural receptors but also a corollary of long-term associated memories (or cues) of substance use and self-administration. Vulnerability to addiction has both physiological and psychological components.
Genetic factors
Contemporary research in the neurobiology of addiction points to genetics as a major contributing factor to addiction vulnerability. It has been estimated that 40–60% of the vulnerability to developing an addiction is due to genetics. One gene in particular, the D2 subtype of dopamine receptor, has been studied at length in association to substance addiction. The D2 receptor responds to the chemical dopamine which produces rewarding and pleasurable feelings in the brain. Through mice studies, agreeing contemporary research has shown that individuals with a deficiency in this dopamine receptor exhibit not only a preference for and increased consumption of alcohol over their genetically normal peers, but also compensated levels of the cannabinoid receptor type CB1. This suggests that both of these genetic factors work together in the regulation of alcohol and cocaine in the brain and in the normal regulation of dopamine.
Additionally, genetics play a role on individual traits, which may put one at increased risk for experimentation with drugs, continued use of drugs, addictions, and potential for relapse. Some of these individual personality traits, such as impulsivity, reward-seeking, and response to stress, may lead to increased vulnerability to addiction.
Environmental factors
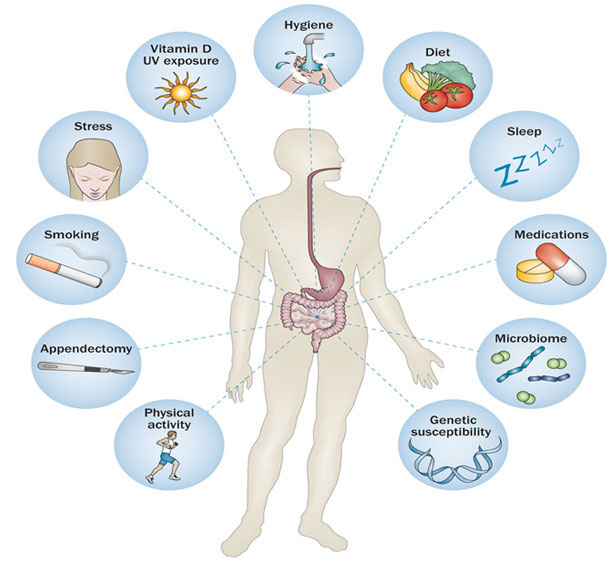
A major environmental factor that increases vulnerability to developing addiction is availability of drugs. Additionally, other environmental factors come into play, such as socioeconomic status and poor familial relationships, and have been shown to be contributing factors in the initiation (and continued use) of drug abuse. Neurobiology again plays a role in addiction vulnerability when in combination with environmental factors. The main risk of chronic stressors contributing to vulnerability is that they can put the brain in a compromised state. External stressors (such as financial concerns and family problems) can, after repeated exposure, affect the physiology of the brain. Chronic stress or trauma has been shown to have neuroadaptive effects such that the brain can essentially physically “rewire” itself to accommodate for the increase in cortisol produced by the stressors. Evidence has also shown that a great amount of stress hinders your prefrontal functioning as well causes an increased limbic-stratal level responding. This can lead to low behavioral and cognitive control.11 Additionally, when the brain is put under severe stress due to repeated drug use, it has been shown to be physiologically altered. This compromised neural state plays a large role in perpetuating addiction and in making recovery more difficult.
Adolescence
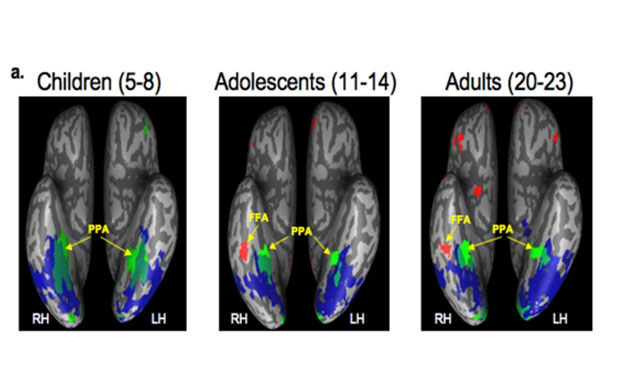
Previous research has examined the increased risk of substance use initiation during adolescence. Many factors have been identified as being associated with increased risk of substance use during this period of development including individual differences (e.g., negative affect, decreased harm avoidance, and low motivation for achievement), biological (e.g., genetic predisposition and neurological development), and environmental factors (e.g., high levels of stress, peer influences, availability of substances, etc.) Rat studies provide behavioral evidence that adolescence is a period of increased vulnerability to drug-seeking behavior and onset addiction. The mesolimbic dopamine system of the brain is undergoing reorganization and functional changes during adolescence. Rat studies have demonstrated that adolescents have tendencies and abilities to drink more than adults due to minimal disruption to their motor functions and also due to minimal sensitivity to sedation.
As a result, it is more susceptible to become addicted in the wake of drug use during this developmental period. Overall, social, behavioral and developmental factors in adolescence make individuals more liable to drug seeking behavior, and as a result, addiction.
Repeated exposure
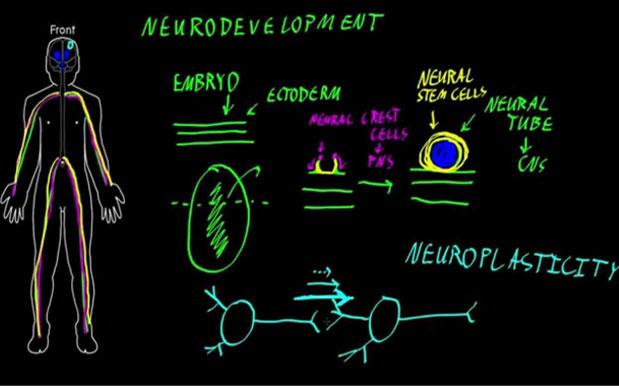
Repeated exposure to a drug is one of the determining factors in distinguishing recreational substance use from chronic abuse. Many neurobiological theories of addiction place repeated or continued use of the drug in the path of addiction development. For example, researchers have theorized that addiction is the result of the shift from goal-directed actions to habits and ultimately, to compulsive drug-seeking and taking. In other words, repeated, deliberate use of the drug plays a role in the eventual compulsory drug-taking and/or habitual drug-taking associated with addiction. Another theory suggests that through repeated use of the drug, individuals become sensitized to drug-associated stimuli which may result in compulsive motivation and desire for the drug. Additionally, a third neurobiological theory highlights the changes in brain reward circuitry following repeated drug use that contributes to the development of addiction such that addiction is conceptualized as being a progression of allostatic changes in which the addicted individual is able to maintain stability but at a pathological set point.
Experience-dependent neural plasticity is a hallmark of repeated drug exposure and refers to the adaptation of the brain due to increased levels of the drug in the body. In this sense, repeated exposure falls under the both physiological vulnerability and behavioral/psychological vulnerability to addiction. Although many variables individually contribute to an increased risk of developing a substance use disorder, no single vulnerability guarantees the development of addiction. It is the combination of many factors (e.g. genetics, environmental stressors, initiation and continued use of the drug) that culminates in the development of this disorder.